Let’s fight breast cancer together
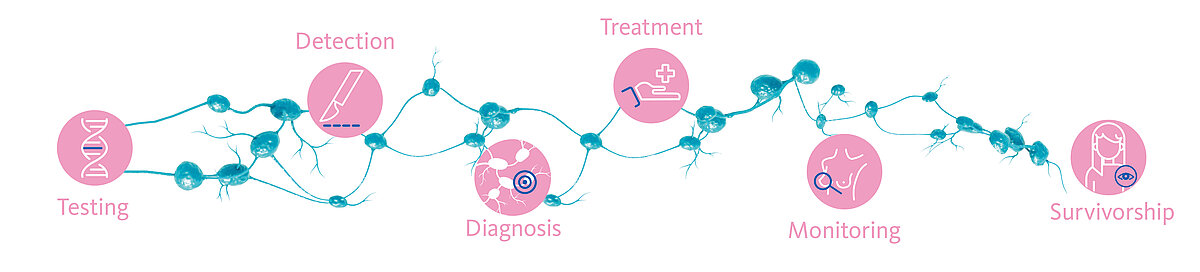
Breast cancer is the most frequently diagnosed type of malignancy in women [1]. Yet, early detection via regular screening and genetic testing for one’s predisposition can increase the chances of making this disease curable and, in several cases, avoidable.
Moreover, the application of new molecular diagnostic tools combined with less invasive surgical approaches and personalised treatments have significantly improved the oncological outcome and patient’s quality of life.
We play a significant role in these improvements, offering a broad portfolio of cutting-edge products spanning the entire breast cancer management process.
The road to the best breast cancer outcomes is paved with information, multi-disciplinary care and personalised oncology.
Prevention
Prevention
Make it a habit. Regularly self-examine to look for any breast lumps, swelling in the axilla region, skin thickening, nipple retraction or blood-stained nipple discharge. Get routine breast imaging depending on your age and potential risk factors. Usually mammography, ultrasound or MRI is used. Knowledge and early detection save lives.
Genetic Testing
Genetic Testing
Everyone has genes that pass along hereditary information from generation to generation. Sometimes changes occur in the gene code, and these changes are called mutations.
In most cases, hereditary breast cancer is due to the presence of a deleterious germline (inherited) mutation in BRCA1 and/or BRCA2 genes [2].
Prior to testing, a person will usually have a risk assessment, in which they meet with a genetic counselor or other health care provider to review factors such as which of their relatives had cancer, what cancers they had, and at what ages they were diagnosed. If the assessment suggests that someone has an increased risk of carrying a harmful BRCA1 or BRCA2 gene variant, the genetic counselor can order the appropriate genetic test, if the individual decides to have genetic testing.
Below are the NCCN’s recommendation for BRCA1 and BRCA2 testing [3]:
- Breast cancer diagnosis at the age of ≤45 years
- Multiple breast cancers: bilateral or ipsilateral
- Breast and ovarian cancer at any age
- Male breast cancer
- Triple-negative (oestrogen receptor negative, progesterone receptor negative and HER2/neu negative) breast cancer diagnosed ≤60 years of age
- Pancreatic cancer at any age
- Two or more relatives (≤50 years old) with breast cancer
- Three or more relatives with breast cancer at any age
- A previously identified BRCA1 or BRCA2 mutation in the family
- Personal history of breast cancer between the age of 46-50 and a close family member with breast, ovarian, pancreatic or prostate cancer
- Personal history of breast cancer at any age and a close family member with breast cancer at age 50 or younger, or two or more close family members with breast cancer at any age
- Metastatic prostate cancer at any age
People who inherit such mutations face high risk of developing breast cancer during their lifetime. Once diagnosed with invasive breast cancer, they carry a high risk of developing a second ipsilateral or contralateral breast cancer [4].
Therefore, a correct diagnosis of the presence of such germline mutations combined with suited prevention and screening strategies are of utmost importance to fight such disease.
Learn how gene mutations can affect breast cancer risk.
Treatment
Treatment
Every treatment order is individual and dependent on the cancer type and stage.
Precision diagnostics for targeted therapy selection in breast cancer – precisely brings to light what needs to be seen
Precision diagnostics are the key to selecting the right therapy at the right time for the right cancer patient.
Gene alterations play a crucial role during the onset and development of breast cancer. Therefore, reliable assessment of the tumour’s mutational status is decisive not only in selecting cancer patients eligible for targeted therapy, but also later in monitoring response to treatment and disease progression.
Nowadays, a range of medications targeting tumour-specific genetic alterations are available and can be prescribed instead of, or in combination with standard chemotherapies, immunotherapies and radiotherapies.
HER2 amplification is seen in approximately 15% of breast cancers and, in the absence of therapy, is associated with a poor prognosis [8,9]. Treatment of patients with HER2 amplification using a specific monoclonal antibody drug has been shown to be effective, increasing overall survival time [10,11].
Furthermore, the FGFR1 gene has been shown to be amplified in approximately 10% of breast cancer patients. It indicates a poor outcome, as over-expression of the gene product has been implicated in early relapse [12-14].
Amplification of TOP2A gene is also seen in breast cancer, frequently with co-amplification of HER2 [15,16]. TOP2A gene aberrations are a marker for the response to anthracycline-based chemotherapy in breast cancer patients [12].
To investigate such genetic changes, oncologists can make use of various molecular genetic tests which may support them in making personalised treatment decisions. Sysmex offers a range of products based on cutting-edge molecular biology technologies, supporting health care professionals and patients along the whole pathway of care.
Therapy selection
With CytoCell® FISH (Fluorescence In Situ Hybridisation) probes* for HER2 (ERBB2), FGFR1, TOP2A, MET, EGFR and RB1 genes, oncologists will get specific information on key druggable genes and prognostic markers.
* CytoCell® FISH probes: For laboratory professional use only. Not intended for use as stand-alone diagnostics or companion diagnostics. Therapeutic action should not be initiated on the basis of the FISH result alone.
Manufacturer and Trademarks: CytoCell® FISH Probes (Cytocell Limited), SureSeqTM myPanelTM (Oxford Gene Technology IP Limited)
Monitoring
Monitoring
Therapy and recurrence monitoring
Despite surgical and/or systemic primary treatment, up to 30% of breast cancer patients still face disease progression. Thus, monitoring patients for therapy response, particularly resistance mutations and tumour recurrence, is of vital importance to secure the best possible long-term outcome for the patient.
In modern personalised oncology, certain somatic gene alterations have emerged as key biomarkers for disease progression, which are detectable in DNA from tumour tissue or circulating tumour-derived DNA (ctDNA) detected in liquid biopsy. At the stage of monitoring, tissue samples are often not available for analysis. However, liquid biopsies can be sampled repetitively with minimal patient distress and has shown to overcome limitations of tissue biopsies, such as missing tumour heterogeneity, inferior sample accessibility and long turnaround time.
Hence, detection of clinically relevant mutations from a simple blood draw enables oncologists to select the most beneficial therapy and monitor the patient’s response to therapy in real time.
Plasma-SeqSensei™ Breast cancer IVD kit is next-generation sequencing-based (NGS) liquid biopsy assays intended for detection of mutations. Built on ultra-sensitive SafeSEQ technology, the PSS IVD kit portfolio aims to set a new standard for absolute determination of mutant molecules (MMs) independent of real sample DNA input, thus offering oncologists a cutting-edge tool to advance personalised oncology. Due to its ability to determine low variant allele frequencies, it is especially useful for minimal residual disease (MRD) detection and other applications requiring sequential measurement like response, recurrence or resistance monitoring.
Survivorship
Survivorship
Facing breast cancer is a life-altering experience for most breast cancer survivors.
On their journey through cancer, they often learn about strength and optimism. They share their experiences to inspire others.
Learn how we inspire hope to those affected by this disease
Read inspiring survivor stories. They share words of inspiration, hope and how their lives have been changed by breast cancer.
References
[1] Sung H. et al. (2021): Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin., 71(3):209-249.
[2] Paluch-Shimon S. et al. (2016): Prevention and screening in BRCA mutation carriers and other breast/ovarian hereditary cancer syndromes: ESMO Clinical Practice Guidelines. Ann Oncol., 27 (5): v103-v110.
[3] National Comprehensive Cancer Network. (2021): . NCCN Clinical Practice Guidelines in Oncology: Genetic/Familial High-Risk Assessment: Breast and Ovarian. V3.
[4] Kotsopoulos J. (2018): Cancers, 10(12), 524. BRCA Mutations and Breast Cancer Prevention.
[5] Pedro L. et al. (2019): Impact of locally administered carboxydextran-coated super-paramagnetic iron nanoparticles on cellular immune function. Small, 15, 1900224.
[6] Kühn F. et al. (2020): A German study comparing standard wire localization with magnetic seed localization of non-palpable breast lesions. In vivo, 34, 1159-64.
[7] Pohlodek K. et al. (2019): Localization of impalpable breast lesions and detection of sentinel lymph nodes through magnetic methods. Eur. J. Radiol., 120, 108699.
[8] Tsai-Pflugfelder M, et al. (1988): Proc Nat Acad Sci ;85:7177-81.
[9] Bofin AM, et al. (2003): Cytopath 2003;14(6):314-9.
[10] Fountzilas G, et al. (2013): BMC Cancer 2013;13:163.
[11] O’Malley, et al. (2009): J Natl Cancer Inst 2009;101(9):644-650.
[12] Letessier A, et al. (2006): BMC Cancer 2006, 6:245.
[13] Courjal F et al., (1997): Cancer Res 1997;57(19):4360-7
[14] Turner N et al., (2010): Cancer Res 2010;70(5):2085-94
[15] Bofin AM, et al. (2003): Cytopath 2003;14(6):314-9.
[16] Fountzilas G, et al. (2013): BMC Cancer 2013;13:163